Bunions affect millions worldwide, causing pain and discomfort that can significantly impact daily activities.
These bony bumps, which form at the base of the big toe, develop gradually, often due to wearing tight shoes or having certain foot structures.
Living with bunions doesn’t have to mean living with pain. There are many ways to manage bunion discomfort, from conservative treatments like proper footwear and orthotic devices to advanced surgical options.
Understanding these options is crucial for making informed decisions about your foot health and preventing the progression of this common condition.
Key Takeaways
- Proper footwear choices and early intervention can significantly slow bunion progression and reduce pain.
- Before considering surgical options, Conservative treatments like padding, orthotics, and physical therapy should be tried.
- Regular foot care and consultation with a podiatrist are essential for effective bunion management and preventing complications.
Understanding Early-Stage Bunion Development
Recognizing bunions in their early stages provides the best opportunity for non-surgical intervention and progression prevention.
Early detection involves identifying subtle changes in foot alignment and addressing contributing factors before significant deformity occurs.
Early Warning Signs
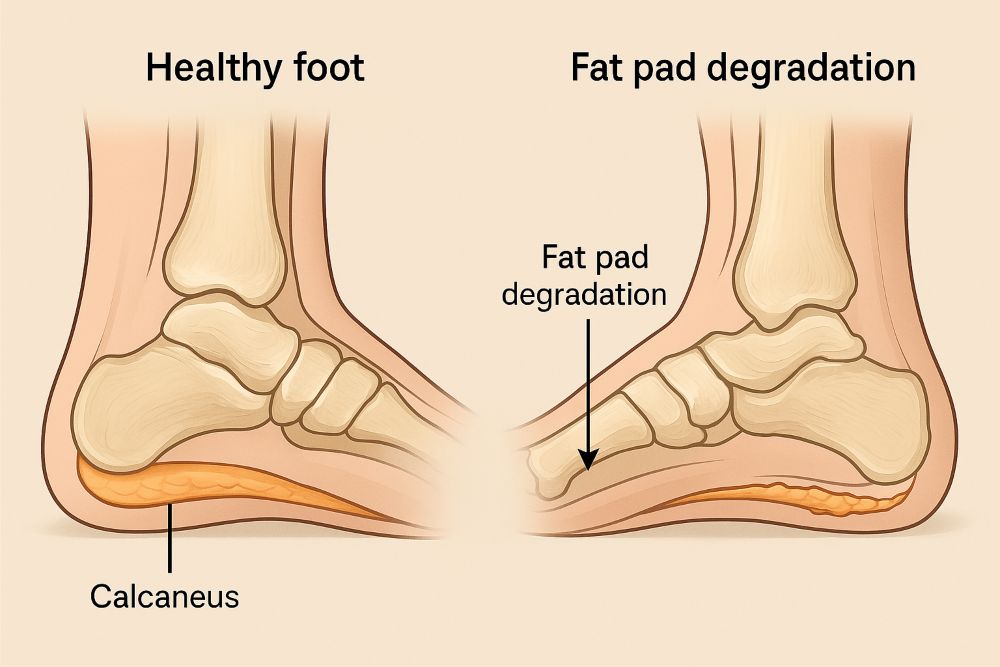
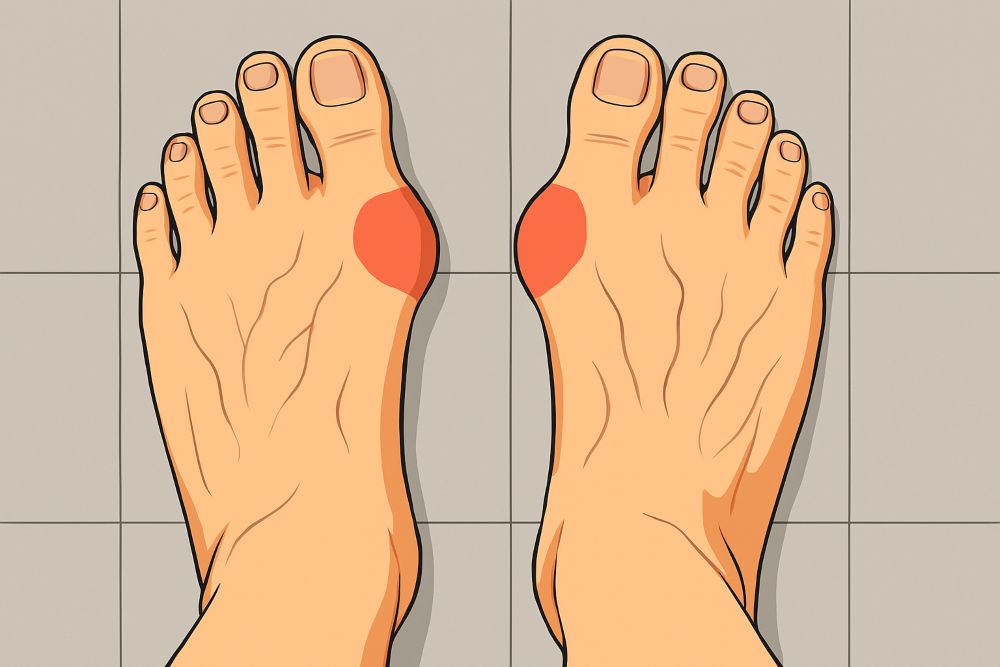
The initial development of a bunion, medically known as hallux valgus, often begins with subtle changes at the metatarsophalangeal joint.
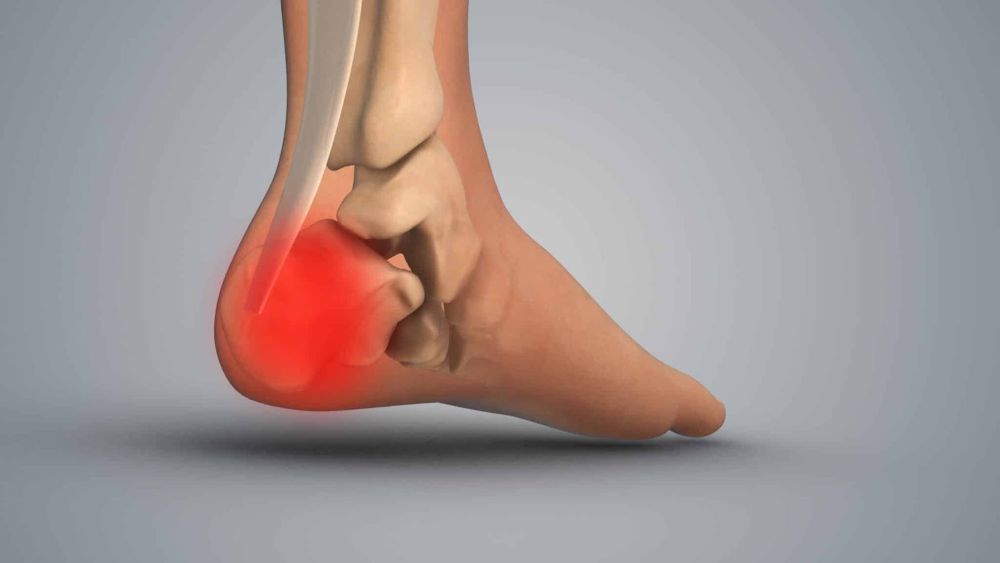
Patients may notice a slight bump forming at the base of the big toe, accompanied by mild redness or tenderness.
Early-stage bunions typically present with the big toe beginning to angle toward the second toe, widening the forefoot. This deviation may be more noticeable when standing or walking.
Key early indicators include:
- Mild discomfort when wearing closed-toe shoes
- Slight inflammation around the first metatarsal head
- Redness without significant pain
- Difficulty finding comfortable footwear
Many make the mistake of early bunion formation for normal foot shape variations or blame it on shoe pressure alone. However, even minor changes warrant attention to prevent progression.
How to Prevent Bunions from Getting Worse
Slowing or preventing the progression of bunions involves a comprehensive strategy aimed at minimizing stress on the metatarsophalangeal (MTP) joint.
Early intervention and consistent foot care can significantly reduce discomfort and help maintain normal foot function.
Smart Footwear Choices
Proper footwear is one of the most effective measures for preventing bunion development and reducing symptoms. Shoes should be carefully selected with the following features:
- Wide toe box – Allows natural toe splay and reduces crowding or overlapping of the toes.
- Low heel (under 2 inches): This shoe minimizes pressure on the forefoot and decreases strain on the MTP joint.
- Soft, breathable materials – Prevent excessive friction and compression across the bunion area.
- Appropriate arch support – Supports the foot’s natural shape and promotes proper weight distribution.
Orthotic Support
Custom orthotics are highly beneficial in bunion prevention and management, particularly for individuals with flat feet or abnormal gait patterns. These prescription shoe inserts provide:
- Enhanced stability
- Targeted pressure relief at the big toe joint
- Improved foot alignment during standing and ambulation
Nighttime Aids and Daily Monitoring
Additional tools may support joint positioning and symptom relief:
- Toe spacers – Worn between the first and second toes to reduce overlapping and encourage better alignment.
- Bunion splints are often used overnight to gently realign the big toe; their effectiveness can vary depending on individual anatomy and severity.
Routine self-examinations and professional foot evaluations are important to detect early joint structure or alignment changes. Monitoring the feet regularly allows for timely intervention before the deformity worsens.
Looking for long-lasting relief from bunion pain? Discover how the Foot, Ankle & Leg Vein Center’s Lapiplasty® 3D Bunion Correction™ can restore comfort and balance to your stride.
Comprehensive Lifestyle Modification Guide
Managing early bunion development requires consistent lifestyle adaptations that support foot health.
Weight management is essential as excess body weight increases pressure on the forefoot, potentially accelerating bunion formation.
Daily foot care practices:
- Gentle foot stretches targeting the big toe joint
- Ice application after long periods of standing/walking
- Foot soaks with Epsom salt to reduce inflammation
- Massage techniques for the arch and forefoot
Activity modifications may include limiting high-impact exercises that place excessive force on the forefoot. Swimming and cycling provide excellent cardiovascular benefits with minimal foot stress.
Workplace adjustments like using ergonomic floor mats and taking regular breaks from standing can prevent excessive pressure on the metatarsal heads. Home habits should include avoiding barefoot walking on hard surfaces.
The Role of Genetics in Bunion Development
Genetics plays a significant role in bunion formation, with family history being one of the strongest predictors of early-onset cases.
Inherited Foot Structures That Contribute to Bunions
Certain biomechanical traits passed down through families can predispose individuals to bunion formation, including:
- Flat feet (fallen arches) – Reduces natural shock absorption and alters foot mechanics
- Excessive pronation – Causes the foot to roll inward excessively, stressing the first metatarsophalangeal (MTP) joint
- Ligamentous laxity – Loose ligaments allow for joint misalignment over time
- Abnormally long or short metatarsal bones – Alter pressure distribution across the forefoot
- Low transverse arch – Reduces structural support at the ball of the foot
.
These inherited structural traits disrupt normal gait mechanics, increasing stress on the big toe joint and contributing to bunion formation over time.
Why Genetic Awareness Matters
Recognizing a genetic predisposition allows for earlier intervention. Before symptoms appear, individuals with a strong family history of bunions should consider preventive strategies, such as supportive footwear, custom orthotics, and routine foot monitoring.
Early action can help preserve joint alignment and delay or even prevent the need for surgical correction.
Are you worried your bunion is getting worse? Schedule a personalized evaluation with the Foot, Ankle & Leg Vein Center to see if custom orthotics can ease pressure and protect your foot alignment.
Exercise and Physical Therapy for Bunion Management
Targeted exercise and physical therapy can help slow the progression of bunions by improving foot strength, alignment, and mobility.
These conservative approaches help offload pressure from the first metatarsophalangeal (MTP) joint and support optimal biomechanics during movement.
Strengthening the Right Muscles
When practiced consistently, foot-specific exercises can reinforce the intrinsic muscles responsible for stabilizing the big toe and arch.
Recommended exercises include:
- Toe spreads and resistance band grips – Strengthen small stabilizing muscles and promote natural toe alignment
- Marble pickups – Engage the short flexor muscles of the toes, enhancing control and dexterity
- Towel scrunches – Activate the plantar muscles and improve arch integrity
- Great toe extensions with resistance – Target the extensor hallucis longus to counteract inward drift
- Ankle strengthening exercises – Improve overall foot and ankle stability, reducing compensatory movements
Physical Therapy Interventions
A licensed physical therapist may incorporate several specialized techniques to optimize outcomes:
- Manual therapy – Hands-on mobilization to improve joint range of motion, particularly at the MTP joint
- Gait analysis – Assessment of walking patterns to identify biomechanical abnormalities; therapists may recommend footwear adjustments, orthotics, or retraining techniques.
- Modalities – Use of ultrasound or electrical stimulation to reduce inflammation and enhance tissue healing around the bunion
- Functional retraining – Education on proper foot mechanics during everyday activities to avoid further stress on the forefoot
Flexibility and Mobility Maintenance
Maintaining flexibility in the lower leg and foot is essential for healthy movement mechanics. Specific strategies include:
- Achilles tendon and calf stretches – Improve ankle dorsiflexion and reduce compensatory forefoot loading
- Sesamoid bone mobility exercises – Help preserve motion beneath the first metatarsal head, supporting efficient toe-off during gait.
By integrating strengthening, flexibility, and therapist-guided interventions, patients can proactively manage bunion symptoms and minimize progression, often delaying or avoiding surgical intervention altogether.
Conclusion
Bunions may develop gradually, but their impact on mobility and comfort can be significant if left unaddressed.
Fortunately, early recognition and a proactive approach can go a long way toward managing symptoms and slowing progression—often without surgery.
Every small step, from choosing the right footwear and using custom orthotics to incorporating targeted exercises and physical therapy, contributes to long-term foot health.
Individuals with a genetic predisposition or early-stage signs should be especially vigilant and begin preventative care as soon as possible.
The key is consistency and awareness. By combining lifestyle changes with professional guidance, you can protect your feet, maintain daily comfort, and stay active without bunion-related limitations.
Consult with a podiatrist or foot specialist to develop a personalized management plan and control your bunion care before it affects your quality of life.
Don’t wait until walking becomes painful. Contact the Foot, Ankle & Leg Vein Center today and take the first step toward lasting bunion relief with advanced bunion surgery options.
Frequently Asked Questions
What is the main cause of bunions?
Bunions are most commonly caused by inherited foot structures that affect biomechanics, such as flat feet, excessive pronation, and joint hypermobility. Poor footwear choices, like narrow or high-heeled shoes, can worsen the condition.
Can bunions go away without surgery?
No, bunions do not go away on their own. However, non-surgical treatments like orthotics, physical therapy, proper footwear, and lifestyle changes can reduce pain and slow its progression.
How can I prevent bunions from getting worse?
To prevent bunion progression, wear wide-toe shoes with proper arch support, avoid high heels, use custom orthotics, perform foot-strengthening exercises, and monitor foot alignment regularly.
Is bunion development hereditary?
Yes, bunion development has a strong genetic component. Traits like flat feet, loose ligaments, or abnormal bone structure can be inherited, increasing the likelihood of bunion formation.
Do bunion splints and toe spacers work?
Bunion splints and toe spacers may help improve alignment and relieve mild symptoms, especially when used early. However, their effectiveness varies, and they do not correct the underlying deformity.
Which exercises help manage bunions?
Toe spreads, marble pickups, towel scrunches, and resistance-based big toe extensions help strengthen intrinsic foot muscles and support toe alignment, reducing bunion-related strain.
When should I see a podiatrist for a bunion?
See a podiatrist if you notice a bump at the base of your big toe, have consistent pain, or experience difficulty finding comfortable footwear. Early evaluation helps avoid worsening deformity.