Have you ever noticed your feet hurt more now than they did years ago? As we age, the protective fat pads in our feet naturally break down, causing pain and discomfort.
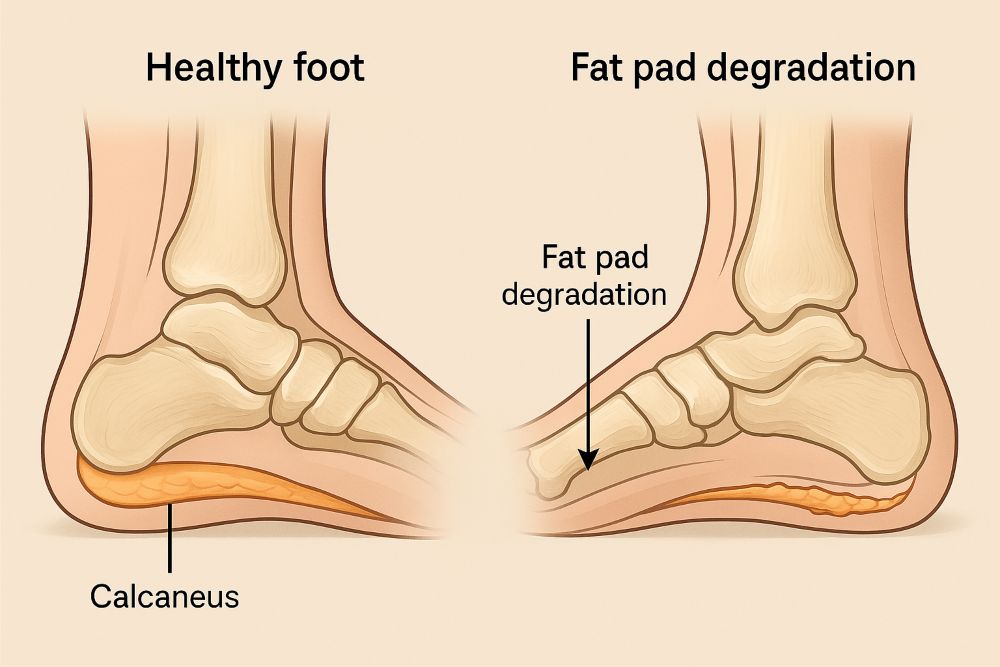
Fat pad atrophy is the gradual breakdown of fat tissue that doesn’t repair or reverse with time. This leaves foot bones closer to the floor and reduces natural shock absorption.
This condition affects many people as they age, but few understand what’s happening. The fat pads on our feet are natural cushions, protecting bones and joints from impact when walking.
When these pads begin to degrade, even simple activities like standing or walking can become painful experiences.
Understanding the early signs can help you seek treatment before the problem worsens.
Key Takeaways
- Fat pad atrophy occurs when protective foot cushioning breaks down with age, causing pain and reduced shock absorption.
- Common symptoms include increased foot discomfort, callus formation, and difficulty walking on hard surfaces.
- Early detection and proper management with specialized footwear or medical treatments can significantly improve comfort and mobility.
Understanding Age-Related Changes in Foot Fat Pads
The protective fat pads in our feet naturally thin over time due to biological processes and external factors.
These changes affect how our feet absorb shock and can lead to discomfort when walking or standing.
The Body’s Natural Breakdown Process
As we age, the fat tissue in our feet deteriorates through fat pad atrophy. This condition involves the breakdown of fat tissue that doesn’t repair itself over time.
The result is less cushioning between foot bones and the ground.
Several factors can accelerate this natural process:
- Regular wear and tear from daily activities
- High-impact exercise that puts repeated stress on the feet
- Certain footwear choices, especially those lacking proper support
- Obesity, which adds extra pressure on the fat pads
Research shows that the elasticity of foot fat pads decreases with age, making them less effective at absorbing shock.
This degradation moves foot bones closer to the floor, leaving them less protected during walking and standing.
Hormones and Their Role in Fat Pad Health
Hormonal changes significantly impact fat pad health as people age. Declining estrogen levels in women, particularly after menopause, can accelerate the thinning of protective fatty tissue beneath the skin.
Decreased growth hormone production affects the body’s ability to maintain and repair tissues, including foot fat pads, in both men and women. This hormonal shift contributes to the progressive nature of fat pad atrophy.
Other hormonal factors affecting foot fat pads include:
- Cortisol fluctuations can break down fat tissue
- Thyroid imbalances alter metabolism and tissue maintenance
- Insulin resistance potentially affects fat distribution
These hormonal changes and the natural aging process explain why many people experience increased foot discomfort as they age.
The degeneration of muscle and fat in the feet can cause significant pain when left unaddressed.
Pain from thinning foot pads isn’t just part of getting older. With the Foot, Ankle & Leg Vein Center’s personalized care, there’s real relief ahead. Call our office and take the first step.
The Progression of Fat Pad Degradation
The fat pads beneath our feet naturally change through a predictable sequence of events. These changes affect daily comfort and mobility as protective cushioning diminishes.
From Subtle Shift to Structural Breakdown
Fat pad degradation typically begins with barely noticeable thinning that progresses gradually over the years. Initially, people may experience mild discomfort after long periods of standing or walking.
The fat tissue breakdown does not repair or reverse with time as the condition advances. The protective cushioning becomes increasingly compromised, leading to more persistent foot pain.
In advanced stages, the footpad can decrease by up to 40% of its original thickness. This significant loss means the foot bones move closer to the floor, directly impacting the bone and ground with each step.
X-rays often show visible changes in the final stages, with reduced distance between foot bones and the walking surface.
What Increases Your Risk?
Several factors can accelerate fat pad degradation:
- Age: Natural loss of elasticity and tissue volume occurs after age 40
- High-impact activities: Running on hard surfaces or jumping sports
- Footwear choices: Consistently wearing high heels or shoes without proper cushioning
- Medical treatments: Cortisone injections interfere with natural healing processes, potentially accelerating tissue breakdown
Prolonged weight-bearing activities significantly contribute to faster deterioration. People who stand for work or exercise extensively on hard surfaces face higher risks.
Certain foot structures, particularly high arches or flat feet, create abnormal pressure distributions, leading to uneven fat pad wear over time.
The Physical Toll on Feet and Function
Fat pad atrophy creates significant physical challenges that affect daily comfort and movement. As protective cushioning diminishes, pain develops, and mobility becomes increasingly difficult with each step.
How Pain Begins and Persists
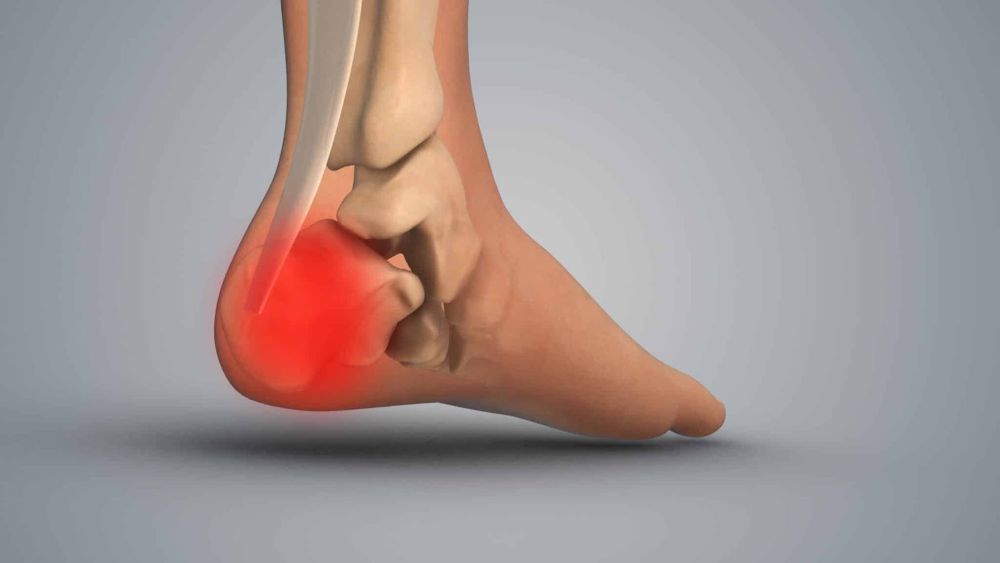
Fat pad degradation means your foot bones come closer to the floor, lacking the natural shock absorption they once had. This creates direct pressure on sensitive structures not designed for such impact.
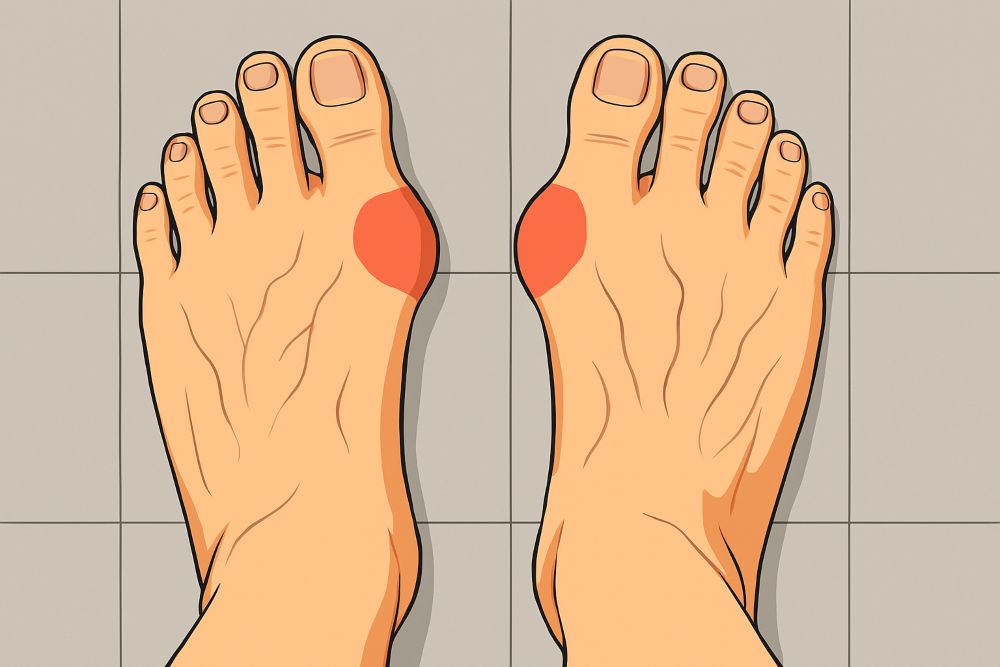
Pain typically begins as a burning sensation under the ball of the foot or heel. Many describe it as walking “directly on bone,” which is essentially what’s happening as the protective fat tissue breaks down.
The discomfort often worsens throughout the day, especially after:
- Long periods of standing
- Walking on hard surfaces
- Wearing shoes without proper cushioning
Unlike temporary foot pain, this condition doesn’t improve with rest alone. The structural change means pain becomes a persistent companion with each step.
Reduced Mobility and Functional Decline
As fat pad atrophy progresses, many people begin limiting activities to avoid pain. This creates a troubling cycle of decreased physical function.
Daily tasks become challenging when every step hurts.
Prolonged walking or standing becomes uncomfortable, forcing modifications to routine activities.
People often develop altered walking patterns to avoid pressure on painful areas. These compensations can lead to:
- Muscle imbalances
- Knee and hip problems
- Increased fall risk in older adults
The impact on quality of life is significant. Social activities, exercise routines, and even basic household tasks may be curtailed. Many report feeling “older than their years” as their activity level declines.
If every step feels thinner, it’s time for a change. Let the Foot, Ankle & Leg Vein Center assess your foot health and help you take pressure off where it hurts most. Schedule your appointment.
How Fat Pad Loss Affects Quality of Life
Fat pad atrophy significantly impacts daily living as protective cushioning diminishes beneath the feet.
This loss of natural padding creates physical limitations and emotional challenges many people don’t anticipate until they experience them firsthand.
Everyday Tasks Become Challenging
When fat pad deterioration occurs in the feet, simple activities that most take for granted become painful ordeals.
Standing for more than a few minutes in the kitchen can trigger shooting pain. Walking on hard surfaces feels like stepping directly on bone, as there’s less cushioning to absorb impact.
Shopping trips often require strategic planning around available seating. Many individuals report needing to:
- Take frequent sitting breaks
- Limit time spent on feet
- Avoid certain flooring types (especially tile and concrete)
Workplace productivity may decline as discomfort increases throughout the day. Some people find themselves unable to maintain jobs requiring prolonged standing.
Physical intimacy and recreational activities can also suffer as pain becomes a constant companion.
The Emotional Side of Aging Feet
The psychological impact of fat pad atrophy extends far beyond physical discomfort.
Many people experience frustration when previously enjoyable activities become sources of pain. Walking with friends, dancing, or playing with grandchildren may be limited.
Social withdrawal often occurs as mobility decreases. When every step hurts, the motivation to attend gatherings diminishes.
This isolation can lead to:
- Feelings of loss and grief
- Decreased self-confidence
- Higher risk of depression
Body image concerns may emerge as special footwear becomes necessary. Many report feeling “old before their time” when foot pain forces lifestyle changes.
The chronic nature of fat pad loss creates an ongoing emotional burden that’s frequently overlooked in medical discussions.
Conclusion
Early detection of fat pad atrophy can significantly improve treatment outcomes and quality of life. Recognizing the signs before severe degradation occurs allows for preventative measures that may slow the process.
Many overlook initial foot pain, attributing it to normal aging or temporary discomfort. This delay often leads to worsened conditions and more limited treatment options.
Various factors, such as cortisone treatments, can cause fat pad atrophy, interfering with natural healing processes. Understanding these risks helps patients make informed decisions.
Regular foot examinations become increasingly important as people age. Healthcare providers can identify early signs of degradation before symptoms become problematic.
Management strategies for fat pad atrophy focus on alleviating symptoms and preventing further deterioration. The earlier these strategies are implemented, the more effective they are.
Remember that prevention is always preferable to treatment. Maintaining a healthy weight, avoiding high-impact activities on hard surfaces, and using proper footwear can help preserve foot pad integrity for longer.
Start reclaiming your comfort today. At the Foot, Ankle & Leg Vein Center, we offer proven solutions for painful fat pad loss so you can walk farther, stand longer, and live fuller. Book your visit now.
Frequently Asked Questions
What are fat pads in the feet?
Fat pads are natural cushions located under the heel and forefoot. They absorb shock, protect bones, and distribute pressure while walking or standing.
Why do foot fat pads wear down with age?
As we age, collagen and elastin levels decline, reducing the thickness and elasticity of the fat pads. Hormonal changes and repeated stress on the feet also contribute to gradual degradation.
What are the symptoms of fat pad atrophy in the feet?
Common symptoms include heel or forefoot pain, burning sensations when walking, feeling like you’re walking on bone, or increased tenderness when barefoot on hard surfaces.
Can fat pad loss cause chronic foot pain?
Yes, without the cushioning from fat pads, more pressure is placed directly on bones and joints, often leading to chronic pain in the heel or ball of the foot.
Is fat pad degradation reversible?
Fat pad loss isn’t reversible, but symptoms can be managed. Orthotics, cushioned footwear, padding, and lifestyle changes can reduce pain and improve mobility.
Who is most at risk for fat pad loss in the feet?
People over 40, especially those with high-impact lifestyles, poorly fitted shoes, or medical conditions like diabetes or arthritis, are more prone to fat pad atrophy.
How can I protect my fat pads as I age?
Wear supportive shoes, avoid walking barefoot on hard surfaces, use cushioned insoles, maintain a healthy weight, and get regular foot checkups to monitor early signs of fat pad thinning.